KNEE ANATOMY AND FUNCTION
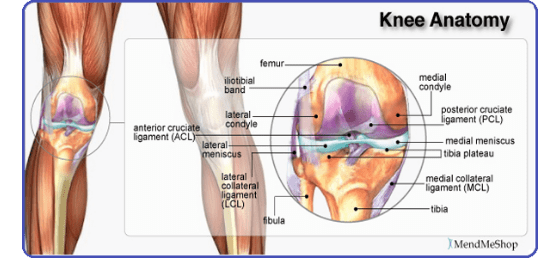
The Knee Joint is made of:
- Bones – Femur, Tibia, Patella & Fibula.
- Ligaments connecting the bones.
- Articular Cartilage which is a coating on the bone like the paint on the wall.
- Menisci – shock absorbers between two bones (femur and tibia) to minimize friction.
- Capsule – covering or encapsulating the joint such that it is a watertight structure.
Muscles outside this capsule which make the joint move
BONES
The Knee Joint is made of the thigh bone (femur) which sits on the leg bone (tibia). In front of both is a knee cap (patella). A thin bone adjacent to the tibia provides structural support.
The Knee thus comprises of three compartments:
Medial Tibiofemoral – the space between the femur and tibia towards the inner side (adjacent to the other leg).
Lateral Tibiofemoral – the space between the femur and tibia towards the outer side (away from the other leg)
Patellofemoral – the space between the femur and the kneecap
Arthritis typically reduces the medial tibiofemoral space to start with. It gradually affects other compartments. Severe arthritis is thus termed tricompartmental i.e. involving all three compartments.
LIGAMENTS
The Knee Joint is made of the thigh bone (femur) which sits on the leg bone (tibia). In front of both is a knee cap (patella). A thin bone adjacent to the tibia provides structural support.
Ligaments are strands of soft tissue which connect two bones. They cannot contract or expand and thus are a constant length. They provide stability to the knee. The chief ligaments of clinical importance in Knee injuries are: The Anterior Cruciate Ligament – at the front of the knee. This is one of the most common ligament ruptures following injuries in sports or road traffic accidents. Major advancements over the last 15 years have enabled us to understand these injuries better and treat them by advanced arthroscopic techniques. The Posterior Cruciate Ligament – at the back of the knee. This is a very strong ligament preventing the tibia from moving excessively backwards beneath the femur. Traditionally, this ligament was left to heal by itself. However, results were suboptimal in quite a few cases. Over the last decade techniques (which require a high degree of skill) have evolved in successfully reconstructing this ligament in a subset of patients which would otherwise not do well. The Lateral Collateral Ligament (Posterolateral Complex : PLC) – on the outer side i.e. away from the opposite leg. This ligament complex was unrecognized until a few years ago!! Cruciate ligament reconstructions are liable to fail if this injury goes unrecognized. Reconstruction of this ligament complex is one of the most recent advancements in knee ligament reconstructions.
The Medial Collateral Ligament – on the inner side i.e. towards the other leg. Sprains of this ligament are very common. Complete tears do pose a treatment dilemma especially when they are associated with other ligament injuries.
The Patellofemoral Ligament – This ligament connects the kneecap to the femur. Recurrent kneecap dislocations (especially after an injury) cause it to rupture. Reconstruction of this ligament is a part of some patellofemoral stabilizations.
ARTICULAR CARTILAGE
This is the smooth coat of white tissue over the femur, tibia and patella which reduces friction between opposing bones. Erosion of this coating results in irregular surfaces rubbing against each other – Arthriti
This phenomenon might affect very small areas in the young athletic adult. Such defects are called Osteochondral Defects and are amenable to Articular Cartilage Restoration procedures.
Erosion of articular cartilage might affect just one compartment of the knee. Such knees respond well to Joint Realignment procedures or Limited Replacements.
Wide erosion of cartilage results in severe arthritis. Such knees respond well to Total Knee Replacements.
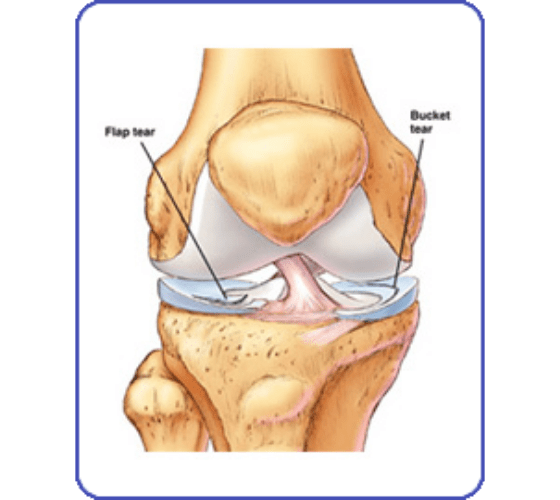
MENISCUS
Besides the articular cartilage, there are two shock absorbers which prevent the femur from rubbing against the underlying tibia. They withstand the impact of the forces across this weight bearing joint. These structures might tear as a result of an injury or as a result of degeneration consequent to arthritis.
Since most of the meniscus (except the outermost portion) has no nourishment from blood vessels, tears do not heal. Peripheral tears in the outermost portion can be stitched by skilled arthroscopic techniques. Other tears need to be excised.
The biomechanics of a meniscus is such that removal of the torn portion restores its weight bearing properties.
CAPSULE
The knee is in a polythene bag – The Capsule. This structure renders the knee water tight.
A contraction of the capsule limits motion. This is generally seen after injury especially when the knee has been immobilized for long periods. It is thus important to follow supervised rehabilitation regimes.
Knees with limited range of motion consequent to contracted capsules are dealt with by arthroscopic releases followed by immediate aggressive physiotherapy.
MUSCLES
The two chief muscle groups are the Quadriceps in the front of the knee and The Hamstrings at the back.
Grafts to reconstruct ligaments are taken from portions of these muscles.
A well coordinated contraction of these muscle groups is important in proper knee motion. Physiotherapists spend most of their time achieving the right balance, flexibility and strength in these muscle groups.
KNEE PAIN MANAGEMENT
Pain Management of the knee involves two chief aspects:
Relieving the pain and consequent agony
Addressing the cause of pain
RELIEVING PAIN
In case of an injury, we advise the RICE regime
R – Rest (Splint the knee or use a good Knee Support)
I – Ice Compresses 10-15 mins each every 4 hours
C – Compression (A Light Compression Bandage)
E – Elevation (Keep the knee on a pillow)
An anti-inflammatory (such as an Aceclofenac & Paracetamol combination) is a good supplement to this therapy.
Patients presenting with painful swollen knees at the clinic gain immediate knee-pain-management relief from the Intermittent Pneumatic Cryotherapy Device. Fluid accumulated in the knee as a result of injury or inflammation is removed and the Cryocuff applied for approximately 20 minutes. This results in dramatic relief of pain and swelling.
Patients presenting with painful knees as a result of mild to moderate arthritis can experience good relief from one of the following injections:
Steroids with Local Anaesthetics : Steroids help in reducing inflammation and thus pain. One or two injections at an interval of a month are acceptable; however, repeated steroid injections might cause more damage than good. Such injections are generally given by Rheumatologists and some Orthopaedic Surgeons in patients suffering from Rheumatoid Arthritis.
Viscosupplementation : These injections consist of substances which replicate lubricating enzymes present in a normal knee. These lubricants reduce friction between the thigh and leg bone in arthritis (which otherwise occurs due to the reduced space between these two bones). Unfortunately, in approximately 50% of patients, their effect weans off in 6-12 months. This is a good way of managing young patients with moderate arthritis or delaying a surgical procedure in the elderly. Pain relief is good. These products can be offered as a one off injection or as weekly injections for 5 weeks.
Manual Physiotherapy Techniques at the Clinic have brought relief to several patients with painful knees. These techniques, popularized by Milligan in the United States, aim at reducing pain by developing coordinated muscle recruitment, stretching unduly taut structures and gentle massages.
ADDRESSING THE CAUSE OF PAIN
Relieving pain is just half the management. It is important to correct the underlying disease.
Simple, specific, graduated, supervised exercises by our Specialist Physiotherapists often start the corrective course. Once self reliant, patients are left to pursue these exercises at home. Quite often, 15 -20 minutes of daily exercises are sufficient to achieve healthy, pain free knees. Such regimes help patients with ligament injuries, muscle weakness, abnormal muscle recruitment or coordination, mild to moderate arthritis, post operative situations, etc. Swimming and Static Cycling work wonders with some knee problems.
In a significant number of patients Viscosupplementation (lubricating enzymes mentioned above) followed by exercises achieves a cure. This is especially useful in patients with mild to moderate arthritis or after a telescopic (arthroscopic) procedure.
Patients with torn ligaments that do not heal (such as the ACL), torn pieces of articular cartilage (loose bodies) floating in the joint, torn shock absorbers (meniscus), inflammation of the knee lining (synovitis), infections or early arthritis where locking and instability are the chief complaints do respond extremely well to simple Telescopic (Arthroscopic) procedures.
Patients in pain because of specific fractures can be treated with arthroscopic and minimally invasive means such that they are up and about on their feet the very next day.
Pain from severe arthritis affecting only a part of the joint can be relieved by Joint Preservation (Joint Realignment & Articular Cartilage Restoration) procedures. Advantages of retaining the patient’s own knee are obvious. Unicompartmental (Limited) Joint Replacements are another option for suitable patients.
Severe arthritis affecting the whole joint requires Total Joint Replacement Surgery. Newer techniques and modern implants have made a tremendous difference in outcomes.

